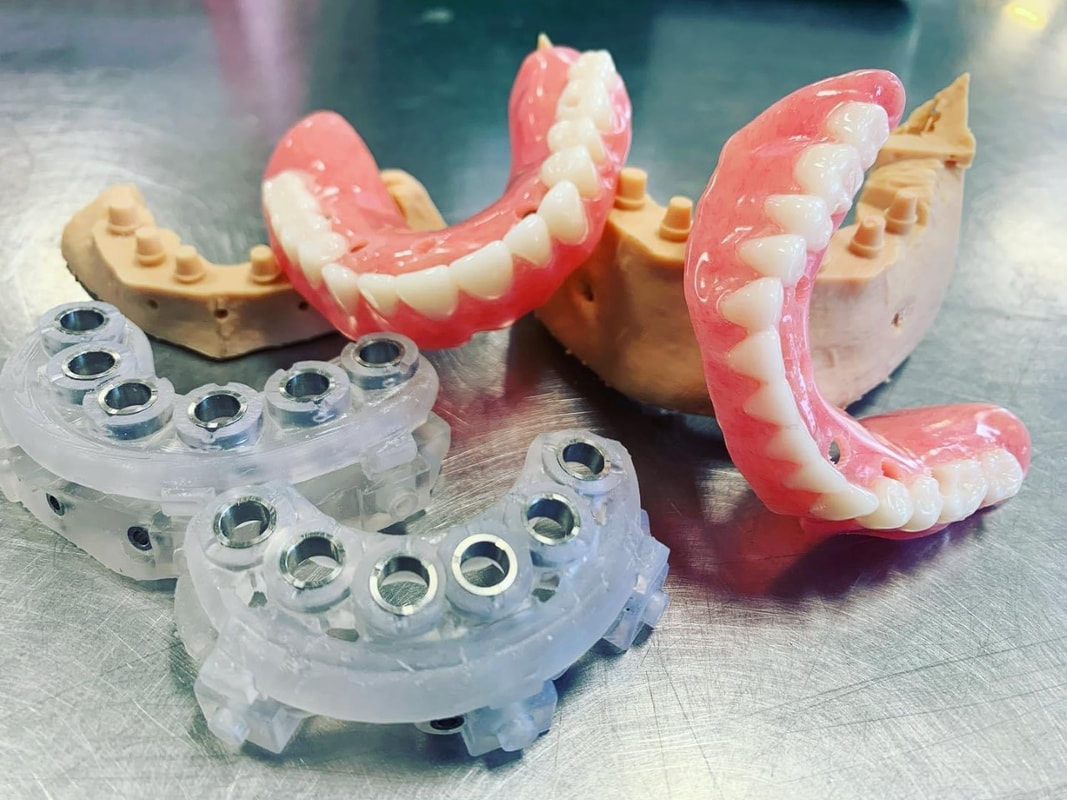
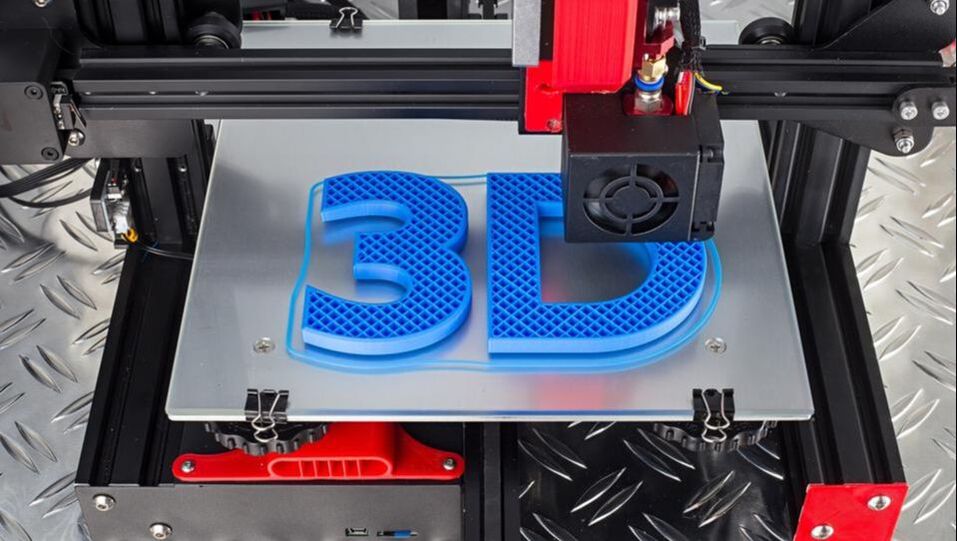
In dentistry, digital guided implant surgery is a procedure to install implants following a template for proper angulation and surgical placement. A surgical guide or template is created using computer-aided design and manufacturing (CAD/CAM) based on computerized tomography (CT) or cone-beam computed tomography (CBCT) scanning. The guide plays an important role in transferring the pre-mapped plans to the implant site. Plans for surgery regarding the implant placement, angulation, depth, and drilling sequence necessary are designed via CAD/CAM software. The computer software provides a 3D image of the edentulous space and serves as a visual aid for proper placement in the bone. It allows the final process to be visualized through virtual design before any surgical intervention, maximizing the smile design and emergence profile of the final prosthesis. Using a surgical guide is a minimally invasive approach to implant surgery that is renowned for accuracy and precision for implant placement. It is favored by patients and doctors because less treatment time is necessary, second-stage implant surgery is not needed, and there is a reduced risk of damage to critical anatomic structures and patient morbidity. CONDITIONS AND INDICATIONS PRIOR TO IMPLANT TREATMENTThere are several conditions and indications that must be considered before planning any dental implant reconstruction. Doctors need to evaluate what kind of materials they need by determining whether the patient is filling space for a single tooth or multiple teeth and whether support is needed for an implant-retained palateless overdenture or partial denture. Any healing problems or uncontrolled medical conditions can impact the survival of the implant. Conditions such as diabetes or immunosuppressive diseases have the potential to affect integration adversely. Moreover, bleeding conditions are not ideal for surgery and may be a contraindication. Medication, such as bisphosphonates can also impact integration and even inhibit the healing of the bone. Additionally, doctors must consider the quantity and quality of hard tissue available as well as adequate vertical and horizontal bone to support the implant. The width of bone should allow at least 1 to 2 millimeters (mm) of facial and lingual cortical bone. The height should be able to support a 1:1 crown-to-root ratio. An adequate gap between the implants, mucosa, and adjacent teeth is necessary for accuracy. Computer-assisted guidance allows <2 mm linear deviation error and angular deviance of <5°. Ideal implant placement consists of outcomes that are aesthetic with optimal occlusion and that are able to maintain the health of peri-implant tissues. Improper positioning can lead to many complications, such as unfavorable mechanical load that can lead to peri-implantitis and implant loss. Additionally, it could lead to other biological complications caused by the inability to maintain proper hygiene. HISTORY OF SURGICAL GUIDESComputerized tomography in medicine has been used since the late 1980s. Initially used for imaging of the human head and neurosurgery, computerized tomography, magnetic resonance imaging, and positron emission tomography were developed for surgical planning and navigation. In the following years, surgical navigation became heavily utilized in the medical field due to the precision it offers. In dentistry, 3D imaging became widespread for presurgical planning and guiding dental implants during surgery. In 1988, D'haese et al. used dental software to interpret computerized tomography axial slices and diagnose and evaluate alveolar ridges. ImageMaster-101 combination software was developed in 1991 to compare dental implant images to cross-sectional images. Surgical guides were officially introduced in the following years to assist in gauging the depth and direction of the osteotomy site. Intraoral scanners were implemented with CBCT scans that enhanced the precision and trueness of digital impressions. Scanning and dental surface registration algorithms were then combined to create a fully digital workflow establishing digital planning and two types of methods for digitally guided implant surgery. TYPES OF GUIDE-ASSISTED IMPLANT SURGERYThere are currently two types of implant surgery guides: static and dynamic navigation. The static process follows a drilling template obtained from computerized tomographic images that guide the depth and direction of the implant bed preparation and placement, allowing for a virtually planned position to be transferred to the implant site. The static guides are created with a digital implant plan, guide-creative software, and additive manufacturing technology. They are used intra-operatively and attached to the adjacent teeth, guiding the drilling of the access hole for the implant. Static uses CT-generated computer-aided design and CAD/CAM, stents with metal tubes, and coordinated instrumentation to place the implants. However, implant positioning cannot be adjusted or altered intraoperatively. Thus, the vital determinant of success is digital planning. The static computer-guided method is commonly used for patients who are fully edentulous. The advantage of static placement is that shorter surgical instruments are needed and the mouth can be viewed on a screen. Clinicians can watch the real-time effect of osteotomy sequential drilling and implant placement. A flap or flapless approach is followed. However, a flapless static approach is common when it comes to surgical implant guides because it results in less bone loss, more preservation of the papilla, and improves aesthetics more efficiently. This method is ideal for the anterior region, when there is no need for augmentation of massive bone or soft tissue, or when strategic teeth can be kept. This is a viable treatment option for rehabilitating the edentulous arch for single, partial, or fully edentulous cases. The implant position in the dental arch can be replicated perfectly with immediate loading available. Having a tissue thickness or an implant site that is adjacent to anatomical structures is helpful with a flapless sGIS approach. Fully or partially guided systems are followed for static implant placement. Both systems include osteotomy preparation using surgical templates and implants, but partial systems are done free-hand. Comparing the two, the 5th International Team for Implantology Consensus Conference found fully guided protocols to outperform partially guided systems. On the other hand, dynamic navigation (DN) uses stereo vision computer triangulation to simplify complex cases as it provides full visual control by directly monitoring the computer screen. The advantage of this approach is the ability to adjust the planned implant positioning intraoperatively. The completely digital workflow is beneficial when it comes to timeliness and efficiency, and eliminates room for human errors. Physicians are able to scan the surgical site, preoperatively plan, and place the implant on a single visit and within a shorter time. DN uses CBCT with fiducials markers to index, virtual planning and calibration, and placement conforming to the 3D image on a navigation screen. Stereovision with natural light cameras that use either passive or active arrays of optical technologies tracks the data for imaging the surgical procedure. The drilling sequence is used for osteotomy preparation and once the bur is placed in the planned position, the implant is then placed. With the arrays positioned extra-orally, the stereo camera is able to control the real-time movements and motion tracking of the drill and placement through patient 3D imaging. Depending on the thickness of keratinized tissue, an open flap or flapless approach may follow. Continuous coordination of the patient, image data, and surgical instrumentation is necessary with this method. DN is used in cases where the mouth opening is limited or restricted, or if the posterior of the jaw region is inaccessible. This is also an ideal process for patients with terminal dentition who cannot keep any strategic teeth. Patients who possess edentulous mandibles are also ideal. Research from Wittwer et al. found immediate implant placement in smooth, wide bone areas to be accurate and safe while exhibiting precision at the coronal and apical portion of the implants. When comparing the two methods–static and dynamic navigation–studies conducted by Kaewsiri et al. and Mischkowski et al. found that neither methods result in a statistically significant difference. However, the dynamic approach is considered to be more accurate in terms of angular deviation but has a slightly higher apical deviation. Due to the higher cost and additional space needed for equipment, dynamic navigation is not an ideal practice in a daily scenario. TREATMENT PROTOCOL FOR COMPUTER-ASSISTED IMPLANT SURGERYDigital technology drastically simplifies implant workflow with consistent predictability and clinical insight based on preoperative planning. The process of digital implant placement consists of four steps: CBCT scanning, software program execution, fabrication of surgical drilling guides, and the surgical procedure. Computerized tomography scanning. 3D images of the jawbone are taken to analyze available bone volume, adjacent teeth structures, mucosal thickness, and maxillary sinus position. In addition, the images help to identify the position of the mandibular canal, incisive canal, and mental foramen. The images are retrieved from either computed tomography or cone-beam computed tomography. CBCT is more favored because it uses a lower dose of radiation and costs less. Digital planning is assessed through either one-scan or double-scan procedures. One-scan uses radiopaque resin with the prosthesis in the patient’s mouth. The second procedure includes a primary scan with the patient wearing the denture and a secondary scan of only prosthesis imaging Software program execution. Computer software programs and CAD/CAM are used to create a digital plan, fabricate the guides, and perform the surgery. The 3D images taken from the CBCT scans are converted to Digital Imaging and Communications in Medicine (DICOM) format where the size of the implants is adjusted to fit the implant placement site. The position and contour of the desired restoration determine the ideal implant size and location in the alveolar bone. Using fiducial markers such as gutta-percha, barium sulfate, or silicone index, the optimal implant position is marked. The software serves as a digital virtual environment that mimics the surgical procedure before the operation occurs. Fabrication of surgical drilling guides. The patient’s bite is registered and upper and lower impressions are taken to be articulated. Surgical guides are fabricated based on the registration and impressions, as well as the digital plan created in step two. They can be digitally fabricated through either additive 3D printing or subtractive milling. 3D printing is a popular choice because of the wide availability of printers and materials, and their low cost. Guides can be fabricated manually as well. There are two types of methods for fabrication: model-based or rapid prototyping. Model-based assesses soft and hard tissue and prosthetic fit. On the other hand, rapid prototyping is stereolithographic, providing digital-based data through intraoral scanning. This method fabricates guides with photopolymerization techniques. Compared to model-based fabrication, rapid prototyping requires fewer manual steps. There are four types of guide-supporting surfaces: tooth-supported, mucosa-supported, bone-supported, and special-supported surgical guides. With tooth-supported surfaces, the remaining teeth are used to support the guide. For completely edentulous patients, the mucosa is used as support. The bone-supported method uses bone after raising the mucoperiosteal flap. Lastly, special-supported guides use mini implants or pins. Surgical guides contain sleeves that are either metallic or not–referred to as an open sleeve. Metal sleeves require wider mesiodistal space and can lead to bone overheating during drilling. The saline irrigation is not able to efficiently prevent friction creation. Open sleeves, however, can minimize overheating because the slot is located on the buccal or lingual side, reducing the inter-arch space and allowing saline irrigation to fall directly on the drill. Guide sleeves are specific to each implant system. Surgical procedure. The surgical guide is fitted in the mouth before the operation and must be adapted and stabilized to the soft tissues or teeth using an index. The drilling sequence to follow is specific to the selected implant system. During the procedure, the sequence must be followed exactly. EXPECTED ADVANTAGEOUS OUTCOMES OF SURGICAL IMPLANT GUIDESConventional implant placement processes use either freehand surgery or laboratory-made surgical guides. However, it is nearly impossible to obtain the ideal position, angulation, and depth without a surgical guide. Even with the guides, inaccuracies often occur during the intraoral scan and in the CBCT image. Compared to digital, conventional approaches result in significant errors when placing implants. The average deviation with surgical guides is more than 1 mm. The evolution of digital technology and apparatus has dramatically reduced the time and cost of surgical planning. Digital also has a higher survival rate and is superior in terms of proper implant positioning and taking into consideration the prosthetic outcomes thanks to virtual planning. Digital implant surgery has been found to result in maximum precision, effectivity, predictability, reliability, and efficiency in implant placement without damaging critical anatomic dental structures. Additionally, the interim prosthesis can immediately be loaded following the implant placement. It is a noninvasive approach that causes less trauma and morbidity while better upholding implant posture. Physicians and their patients are able to void surprises and save chair time with the virtual preoperative plan. In terms of both aesthetics and function, CBCT analysis helps to ensure an outstanding long-term prognosis. HOW CAN THE DENTAL LAB HELP?The Dental Lab in Bristol, Pennsylvania offers services and products for dentists, oral surgeons, and their patients using the most efficient and latest technologies and techniques. Our lab is specialized in implants and creates advanced implant guides that are customized through a dental design tutorial to determine accurate surgical drilling and dental implant placement. Contact us today for more information on our products and services. Sources: Digital Implant Planning and Surgical Guides: Tools for Clinical Success Guided Implant Surgery and Attached Gingiva Fully Digital Workflow for Planning Static Guided Implant Surgery Dynamic Navigation for Dental Implant Surgery Expectation and reality of guided implant surgery protocol using computer-assisted static and dynamic navigation system at present scenario Static or Dynamic Navigation for Implant Placement—Choosing the Method of Guidance Keywords:
The dental lab, implants, digital, cad/cam, computerized tomography, guided surgery, implant placement, digital planning, guides, prosthesis, surgical, surgery, static, dynamic navigation, cbct, surgical guide, digital imaging, software, dicom, scanning, digital guided implant surgery
0 Comments
Leave a Reply. |